PROSTATE CANCER
What is Prostate?
Symptoms of Prostate Cancer
Risk factors for Prostate Cancer
Screening in Prostate Cancer
Treatment of Prostate Cancer
da Vinci Robotic & Laparoscopic surgical techniques
Nerve-Sparing for Erection
What is the Prostate?
The normal prostate is a small gland about the size of a walnut (20 milliliters). It sits under the bladder and in front of the rectum. The urethra -the narrow tube that runs the length of the penis and carries both urine and semen out of the body- runs directly through the prostate. The rectum, or lower end of the bowel, sits just behind the prostate and the bladder (Figure-1).
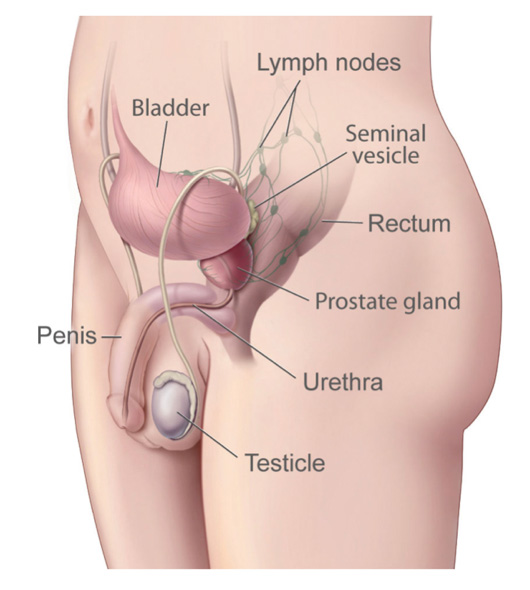
Figure-1: Genitourinary tract in male
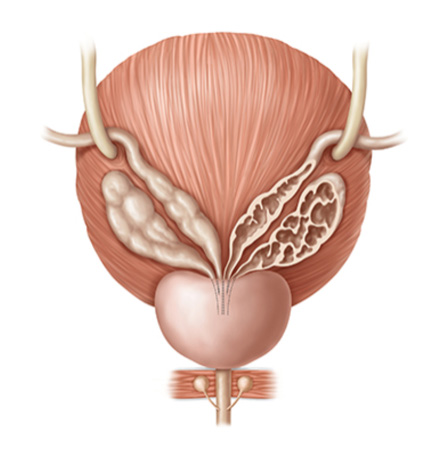
Sitting just above the prostate are the seminal vesicles -two little glands that secrete about 60% of the substances that make up semen (Figure-2). Running alongside and attached to the sides of the prostate are the nerves that control erectile function.
The prostate is not essential for life, but it’s important for reproduction. It seems to supply substances that facilitate fertilization and sperm transit and survival. Enzymes like PSA are actually used to loosen up semen to help sperm reach the egg during intercourse. (Sperm is not made in the prostate, but rather the testes.)
The prostate typically grows during adolescence under the control of the male hormone testosterone and its byproduct DHT, or dihydrotestosterone.
Figure-2: The urethra—the narrow tube that runs the length of the penis and carries both urine and semen out of the body—runs directly through the prostate. Both seminal vesicle with ejaculatory ducts, opening to the urethra.
Symptoms of prostate cancer
Many times, signs of prostate cancer are first detected by a doctor during a routine check-up. Most of the patient do not have urinary tract symptoms. Some men, however, will experience changes in urinary or sexual function that might indicate the presence of prostate cancer. These symptoms include:
- A need to urinate frequently, especially at night
- Difficulty starting urination
- Weak and / or interrupted flow of urine
- Painful or burning urination
- Difficulty in having an erection
- Painful ejaculation
- Blood in urine or semen
- Frequent pain or stiffness in the lower back, hips, or upper thighs. You should consult with your doctor if you experience any of the symptoms above. Because these symptoms can also indicate the presence of other diseases of the prostate as benign prostatic hyperplasia (BPH) or chronic prostatitis, men will undergo a thorough work-up to determine the underlying disease.
Risk factors for prostate cancer
Prostate cancer is the second most common non-skin cancer, affecting 1 in 6 men.
However, who is most at risk of getting prostate cancer and why?
There are several major factors that influence risk, some of them unfortunately cannot be changed.
Age: The older you are, the more likely you are to be diagnosed with prostate cancer. Although only 1 in 10,000 men under age 40 will be diagnosed, the rate shoots up to 1 in 38 for ages 40 to 59, and 1 in 15 for ages 60 to 69.
In fact, more than 65% of all prostate cancers are diagnosed in men over the age of 65. The average age at diagnosis of prostate cancer is about 69 years. After that age, the chance of developing prostate cancer becomes more common than any other cancer in men or women.
Race: African American men are 60% more likely to develop prostate cancer compared with Caucasian men and are nearly 2.5 times as likely to die from the disease. Conversely, Asian men who live in Asia have the lowest risk.
Family history/genetics: A man with a father or brother who developed prostate cancer is twice as likely to develop the disease. This risk is further increased if the cancer was diagnosed in family members at a younger age (less than 55 years of age) or if it affected three or more family members.
In addition, some genes increase mutational rates while others may predispose a man to infection or viral infections that can lead to prostate cancer.
Risk Factors in Aggressive vs. Slow-Growing Cancers
In the past few years, we’ve learned that prostate cancer really is several diseases with different causes. The more aggressive and fatal cancers likely have different underlying causes than slow-growing tumors.
For example, while smoking has not been thought to be a risk factor for low-risk prostate cancer, it may be a risk factor for aggressive prostate cancer. Likewise, lack of vegetables in the diet (especially broccoli-family vegetables) is linked to a higher risk of aggressive prostate cancer, but not to low-risk prostate cancer.
Body mass index, a measure of obesity, is not linked to being diagnosed with prostate cancer overall. In fact, obese men may have a relatively lower PSA levels than non-obese men due to dilution of the PSA in a larger blood volume. However, obese men are more likely to have aggressive disease.
Other risk factors for aggressive prostate cancer include:
Tall height
Lack of exercise and a sedentary lifestyle
High calcium intake
African-American race
Family history
Screening
It’s important for each man to talk with his doctor about whether prostate cancer screening is right for him.
There is no unanimous opinion in the medical community regarding the benefits of prostate cancer screening. Those who advocate regular screening believe that finding and treating prostate cancer early offers men more treatment options with potentially fewer side effects.
Those who recommend against regular screening note that because most prostate cancers grow very slowly, the side effects of treatment would likely outweigh any benefit that might be derived from detecting the cancer at a stage when it is unlikely to cause problems.
A prostate cancer screening may reveal results that prompt a doctor to recommend a prostate biopsy. There are many other supplementary tests and considerations that can help a man who is undergoing screening decide if a biopsy is necessary, including:
- Lower % free PSA
- PSA velocity (rate of rise over time)
- PSA density (PSA per volume of prostate)
- Family history,
- Ethnicity
- Prior biopsy findings such a ASAP or high grade PIN
- Abnormal finding in digital rectal exam
- Different forms of PSA (i.e. bPSA, pro-PSA)
Treatment
A surgical approach to treating prostate cancer will remove all or part of the prostate (Figure-3). Typically, men with early-stage disease or cancer that’s confined to the prostate will undergo radical prostatectomy – removal of the entire prostate gland, plus some surrounding tissue.
Figure-3: Schematic view of the radical prosatatectomy
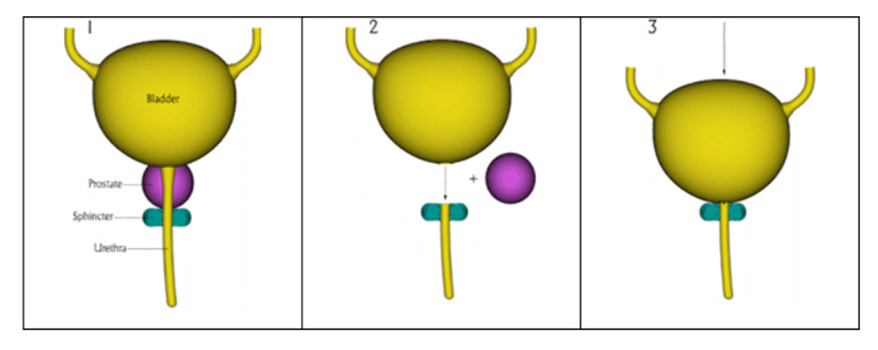
Before 2002, the most common type of prostatectomy was radical retropubic prostatectomy -an incision is made in the abdomen and the prostate is removed from behind the pubic bone- (Figure-4a). The surgeon then stitches the urethra directly to the bladder so urine is able to flow.
In 2010, daVinci robotic radical prostatectomy is the standart surgical approach in the radical prostatectomy due to several advantages including better protection of nerves and vessels for erectile function.
daVinci Robotic & Laparocopic surgical techniques
In laparoscopic and da Vinci robotic surgery, very small incisions are made on the anterior abdominal wall (Figure-4b). The surgeon then inserts narrow instruments fitted with cameras for 3D high definition and 15 times larger view of the surgical field and/or mini-surgical tools, allowing him or her to visualize and operate on the internal structures without cutting open the entire abdomen combining with a good view resulting in better sparing of the erectile vascular and neural structures and all muscles for continence mechanisms.
With a robotic interface, the surgeon maneuvers a robot’s arms, which in turn control the cameras and instruments. Robotic surgery has become very popular over the past 20 years due to the smaller incision and shorter post-operative recovery period.
In the hands of a skilled surgeon, the outcomes of cancer control and side effects are optimized with laparoscopic and da Vinci robotic approaches
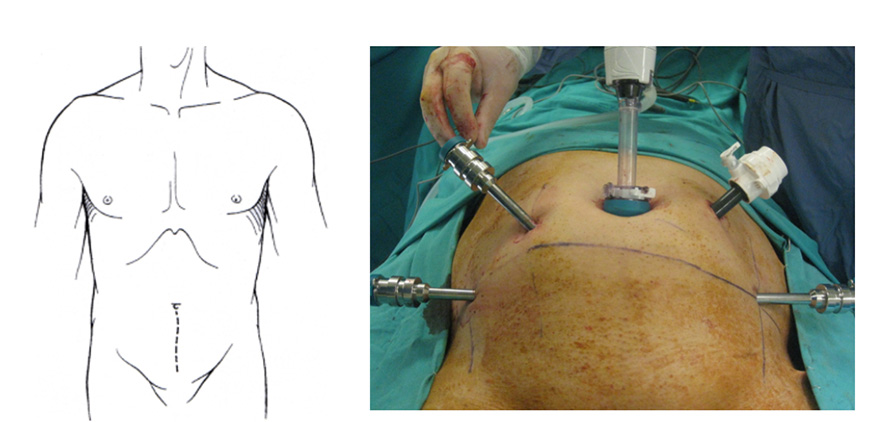
Figure-4: (a) Abdominal insicion for the open radical prostatectomy, (b) mini-punctures for laparoscopic or da Vinci robotic surgery. This trocars for our Extra-Peritoneal Robotic Prostate Surgery locations.
Nerve-Sparing Robotic Surgery for Erection
In a nerve-sparing laproscopic or daVinci robotic prostatectomy, the surgeon cuts to the very edges of the prostate, taking care to spare the erectile nerves and vascular structures that run alongside the prostate. If the nerves cannot be spared because the cancer extends beyond the prostate, it might be possible to surgically attach, or graft, nerves from other parts of the body to the ends of the cut erectile nerves. Hoever, the results is not sufficient with neural grafts.
Open technique surgeon can not know until the time of the procedure if nerve-sparing is possible; it depends on whether the cancer is invading the nerves. However, the nerve-sparing procedure with laparoscopic and daVinci robotic techniques under better visualization with high definition and 15 times larger magnification offers the best chance to preserve long-term erectile function.
In 60’s, erectile function can be preserved in 90-95% of the patients who preoperatively had normal erectile function.
The Importance of Surgical Skill
daVinci Robotic and Laparoscopic Prostatectomy, like many surgical procedures, is very delicate work, and the difference between a good surgeon and a great surgeon can affect outcomes.
When choosing a surgeon, at a minimum, ensure that he is someone in whom you have confidence and trust, and someone who has enough experience to not only perform the operation, but also to make an informed clinical judgment and change course if necessary.
Prof. Dr. Tibet Erdogru has 400 conventional laparoscopic and after the experience with conventional laparoscopic technique, he has 650 robotic radical prostatectomy experience in such challenging cases with larger prostate, obese cases, and after hormonal-chemo therapy.
Treatment-Related Changes
Because the prostate is close to several vital structures, prostate cancer and its treatment strategies can disrupt normal urinary, bowel, and sexual functioning.
Urinary function—Under normal circumstances, the urinary sphincters (bands of muscle tissue at the base of the bladder and at the base of the prostate) remain tightly shut, preventing urine that’s stored in the bladder from leaking out. During urination, the sphincters are relaxed and the urine flows from the bladder through the urethra and out of the body.
During prostatectomy—the surgical removal of the prostate—the bladder is pulled downward and connected to the urethra at the point where the prostate once sat. If the sphincter at the base of the bladder is damaged during the open surgical process, or if it’s damaged during radiation therapy, some measure of urinary incontinence or leakage will occur.
Bowel function—Solid waste that’s filtered out of the body moves slowly down the intestines, and, under normal circumstances, the resultant stool is excreted through the anus following conscious relaxation of the anal sphincter. Damage to the rectum caused by radiation therapy can result in bowel problems, including rectal bleeding, diarrhea, or urgency.
Sexual function—If the erectile nerves are damaged during open radical prostatectomy, which was standard during this type of surgery up until the mid 1980s, the ability to achieve erection is lost. Sexual desire is not affected, but severing or otherwise damaging the nerves can lead to erectile dysfunction. These nerves can also be damaged by radiation, though this process usually occurs much more slowly over time.
Modern techniques in surgery namely nerve-sparing daVinci Robotic Prostatectomy has been developed 15 years ago to minimize these side effects of open surgery, and this process continues to improve our anatomical and functional knowledge. We can say the patient that there will be no incontinence and highly erectile function performance despite the radical prostatectomy if the cancer stage is appropriate for nerve and bladder neck sparing procedure.
Treatment of prostate, bladder, kidney and testicular cancers with robotic and laparoscopic surgery in urology

